Use of Osteochondral Allograft Transplantation for Patellofemoral Cartilage Injury
By: Kirk A. Campbell, M.D.1 and Sanjeev Bhatia, M.D.2
1. NYU Langone Orthopedic Hospital, NYU Langone Health, New York, NY
2. Hip & Knee Joint Preservation Center, Northwestern Medicine West Region, Warrenville, IL
Patellofemoral chondral defects are common and have been reported to account for up to 30-40% of chondral defects in patients undergoing knee arthroscopy.1-3 A majority of these defects are incidental findings, but a significant amount does become symptomatic, causing anterior-based knee pain and swelling. Common causes of patellofemoral chondral damage include patella instability, trauma, osteochondritis dissecans and generalized degenerative changes.3 The complex anatomy of the patellofemoral compartment makes treating these defects quite challenging, due to the morphology of the patella and trochlea, as well as the high joint reaction forces (up to 7.8 times the body weight during deep knee bending and squats). 4,5
There are also a variety of other factors that may add to the complexity of addressing patellofemoral chondral damage, including patellar malalignment; abnormal lateral tilt; instability and maltracking; patella alta or baja; and trochlea dysplasia, to name a few.3,6 A successful surgical approach to addressing any patellofemoral cartilage damage typically also involves concomitantly addressing any underlying pathology with tibial tubercle osteotomy and/or patellar stabilization procedures as needed.

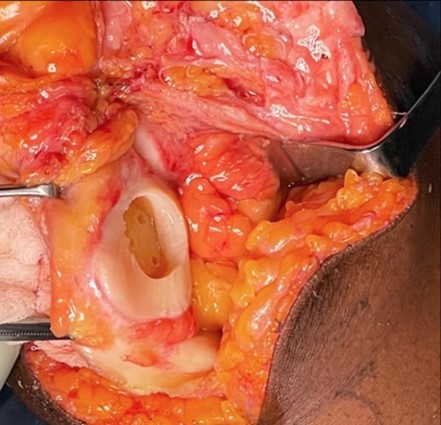
Figure 1: Focal patella cartilage defect found at arthroscopy. There was significant bone marrow edema on MRI.
There are a variety of different approaches that have been used to address symptomatic patellofemoral cartilage defects with varying degrees of success. These modalities have included marrow stimulation techniques (such as microfracture), osteochondral autograft transplantation, matrix-induced autologous chondrocyte implantation (MACI), particulated juvenile cartilage allograft (DeNovo® NT natural tissue graft) and fresh osteochondral allograft (OCA) transplantation. In general, the literature has shown that these techniques have resulted in lower success rates when used in the patellofemoral compartment versus tibiofemoral compartment.3 MACI and OCA transplantation are the two most common methods used to address large symptomatic patellofemoral cartilage defects.
OCA has several advantages over MACI and the other cartilage restoration procedures; it’s also considered to be the go-to salvage procedure for failed cartilage restoration. The use of OCA as a primary procedure for large patellofemoral cartilage defects (>4 cm2) has increased especially for cases with significant subchondral bone marrow edema, osteochondritis dissecans and post-traumatic defects due to its ability to address both the chondral and bone pathology.3,6-8
There are several advantages of OCA; some of these advantages include absence of donor site morbidity, presence of metabolically active chondrocytes and hyaline cartilage with subchondral bone that can be loaded after bone healing. Other advantages include immunoprivilege status, which allows easier graft acceptance, and its ability to be used in revision situations when the subchondral bone has been violated. The unique and varied morphology of the patella and trochlea—including their shape, patella cartilage thickness and surface function—make OCA transplantation more technically demanding.3,6,9 There has been a movement towards using orthotopic grafts, which are grafts emanating from the same anatomic location as the receipt (i.e. use of a patella OCA for a patella defect), in patellofemoral cartilage restoration to address these unique anatomical challenges. However, studies have also shown that use of nonorthotopic grafts can lead to significant short-term improvements in pain and patient-reported outcomes.4,9
Use of OCA for focal patella and trochlea cartilage defects have both resulted in excellent short and mid-term patient-reported outcomes. In one of the largest case series to date of 27 patients (28 knee patients), Gracitelli et al.8 reported that at a mean follow-up of 9.7 years, 89% of patients were extremely satisfied or satisfied with the results of the OCA transplantation. The patella OCA had a survivorship that was 78.1% at five and 10 years and 55.8% at 15 years. However, there was a high (60.7%) reoperation rate and 28.6% failure rate associated with the procedure. For focal trochlea defects, Cameron et al.10 demonstrated that trochlea OCA results in excellent patient-reported outcomes at a mean follow-up of seven years. The graft survivorship was reported to be 100% at five years and 91.7% at 10 years.10 Bipolar cartilage defects are a challenging problem in the patellofemoral compartment. Although bipolar patella and trochlea OCA result in significant improvements in patient-reported functional outcomes and pain relief, they have been found to have high reoperation and failure rates with a five-year graft survival rate of 64.1%.11,12 In a systematic review of OCA for the patellofemoral joint, Chahla et al.6 found that OCA for this challenging problem results in improved patient-reported outcome scores and high patient satisfaction rates. The five and 10-year survival rates were found to be 87.9% and 77.2%, respectively. It is important to correct any underlying abnormalities such as maltracking or instability with concomitant procedures to improve OCA’s success rate.
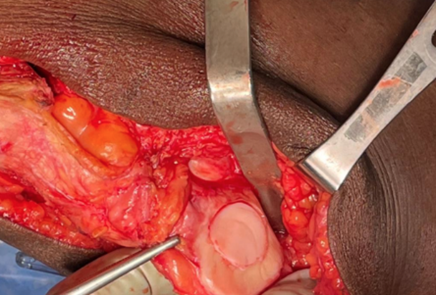
Figures 2A-D: Patella osteochondral allograft transplantation with an orthotopic size matched fresh patella osteochondral allograft and concomitant anteromedializing tibial tubercle osteotomy.
 A.
A.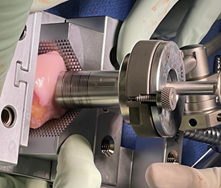 C.
C.
 B.
B. D.
D.
OCA for the patellofemoral joint is a rapidly growing area in cartilage restoration and is an important tool for the sports medicine surgeon to keep in their armamentarium. Keys to success include careful patient selection, use of orthotopic grafts and correcting any underlying abnormalities with concomitant osteotomies or stabilization procedures. More research is needed on the long-term outcomes of OCA for patellofemoral cartilage injury, and we anticipate that the continued increased use of OCA will allow us to answer many of the challenging questions that remain regarding how to best address patellofemoral chondral defects.
References
1. Curl, W.W., Krome, J., Gordon, E.S., Rushing, J., Smith, B.P., Poehling, G.G. "Cartilage Injuries: A Review of 31,516 Knee Arthroscopies." Arthroscopy: The Journal of Arthroscopic and Related Surgery. 1997;13(4):456-460.
2. Lattermann, C., Kremser, V., Altintas, B. "Use of Fresh Osteochondral Allografts in the Patellofemoral Joint." Journal of Knee Surgery. 2018;31(3):227-230.
3. Brophy, R.H., Wojahn, R.D., Lamplot, J.D. "Cartilage Restoration Techniques for the Patellofemoral Joint." Journal of the American Academy of Orthopaedic Surgery. 2017;25(5):321-329.
4. Chahla, J., Hinckel, B.B., Yanke, A.B., et al. "An Expert Consensus Statement on the Management of Large Chondral and Osteochondral Defects in the Patellofemoral Joint." Orthopaedic Journal of Sports Medicine. 2020;8(3):2325967120907343.
5. Flynn, T.W., Soutas-Little, R.W. "Patellofemoral Joint Compressive Forces in Forward and Backward Running." Journal of Orthopaedic & Sports Physical Therapy. 1995;21(5):277-282.
6. Chahla, J., Sweet, M.C., Okoroha, K.R., et al. "Osteochondral Allograft Transplantation in the Patellofemoral Joint: A Systematic Review." American Journal of Sports Medicine. 2019;47(12):3009-3018.
7. Dekker, T.J., Kennedy, M.I., Grantham, W.J., DePhillipo, N.N., LaPrade, R.F. "Patellar Fresh Osteochondral Allograft Transplantation." Arthroscopy Techniques. 2019;8(8):e851-e854.
8. Gracitelli, G.C., Meric, G., Pulido, P.A., Gortz, S., De Young, A.J., Bugbee, W.D. "Fresh Osteochondral Allograft Transplantation for Isolated Patellar Cartilage Injury." American Journal of Sports Medicine. 2015;43(4):879-884.
9. Lin, K.M., Wang, D., Burge, A.J., Warner, T., Jones, K.J., Williams, R.J. "Osteochondral Allograft Transplant of the Patella Using Femoral Condylar Allografts: Magnetic Resonance Imaging and Clinical Outcomes at Minimum Two-Year Follow-Up." Orthopaedic Journal of Sports Medicine. 2020;8(10).
10. Cameron, J.I., Pulido, P.A., McCauley, J.C., Bugbee, W.D. "Osteochondral Allograft Transplantation of the Femoral Trochlea." American Journal of Sports Medicine. 2016;44(3):633-638.
11. Meric, G., Gracitelli, G.C., Gortz, S., De Young, A.J., Bugbee, W.D. "Fresh Osteochondral Allograft Transplantation for Bipolar Reciprocal Osteochondral Lesions of the Knee." American Journal of Sports Medicine. 2015;43(3):709-714.
12. Mirzayan, R., Charles, M.D., Batech, M., Suh, B.D., DeWitt, D. "Bipolar Osteochondral Allograft Transplantation of the Patella and Trochlea." Cartilage. 2020;11(4):431-440.


