Simulation in Arthroscopy Training: Where We Are At, Where We Are Going
By: Niraj V. Kalore, M.D.
Arthroscopic surgery has always included complexities that require substantial hand-eye coordination, manual dexterity and knowledge of anatomy. The learning curve for arthroscopic proficiency can be daunting for the trainee. In an era of cost containment, high volume and added focus on operating room efficiency, time in the operating room is highly constrained. The traditional model of learning in the operating room may not provide enough opportunity to gain the necessary skills. Additionally, the foundational skills of arthroscopy like triangulation and knot tying may not develop sufficiently in the high pressure/high throughput environment the operating room often creates.
Arthroscopy and Simulation: Where Do We Currently Stand?
Since the Accreditation Council for Graduate Medical Education (ACGME) implemented an 80-hour work week rule for residents in 2003, substantial research has focused on simulation to improve arthroscopy training. In a simulated environment, the trainee can focus on perfecting arthroscopic skills without having the added pressure of time or consequences for patient safety. It’s possible to deconstruct complex procedures into specific steps and focus on repeating each step until sufficient proficiency is attained. This strategy can help trainees move up the learning curve more efficiently; supplement traditional teaching; and improve surgeon performance and patient safety.
Modern simulators have expanded training capabilities that range from basic skills like triangulation, knot training and diagnostic arthroscopy to complex meniscus, ligament and tendon repair or reconstructions in the hip, knee and shoulder joints. Benchtop simulators have low fidelity but help improve basic skills like triangulation and knot tying in a simplified environment.
Cadaveric simulation has the benefit of presenting real anatomy and haptic feedback, along with the ability to perform complex reconstruction procedures. However, limited availability and cost reduce the feasibility of this simulation method. Virtual reality simulators are a recent advance where three-dimensional anatomy is virtually simulated, and trainees can practice a range of simple to complex procedures.
AANA has been at the forefront of these significant advances in simulation for arthroscopy training. Under the direction of Robert Pedowitz, M.D., Ph.D., AANA, the American Board of Orthopaedic Surgery (ABOS) and the American Academy of Orthopaedic Surgeons (AAOS) collaborated on creating the Fundamentals of Arthroscopic Surgery Training (FAST) training program and workstation, which is designed to help Orthopaedic Surgeons master triangulation, arthroscopic knot tying and simple procedures like foreign body removal, meniscus debridement and even a rotator cuff repair. The three-dimensional FAST workstation has trained thousands of residents since 2011. The versatile, portable tool, with multiple training modules, is designed to improve the psychomotor skills used in arthroscopic surgery.


The Future of Arthroscopy and Simulation
Orthopaedic surgical training as we know it is on the verge of a paradigm shift, and AANA is quickly catching on.
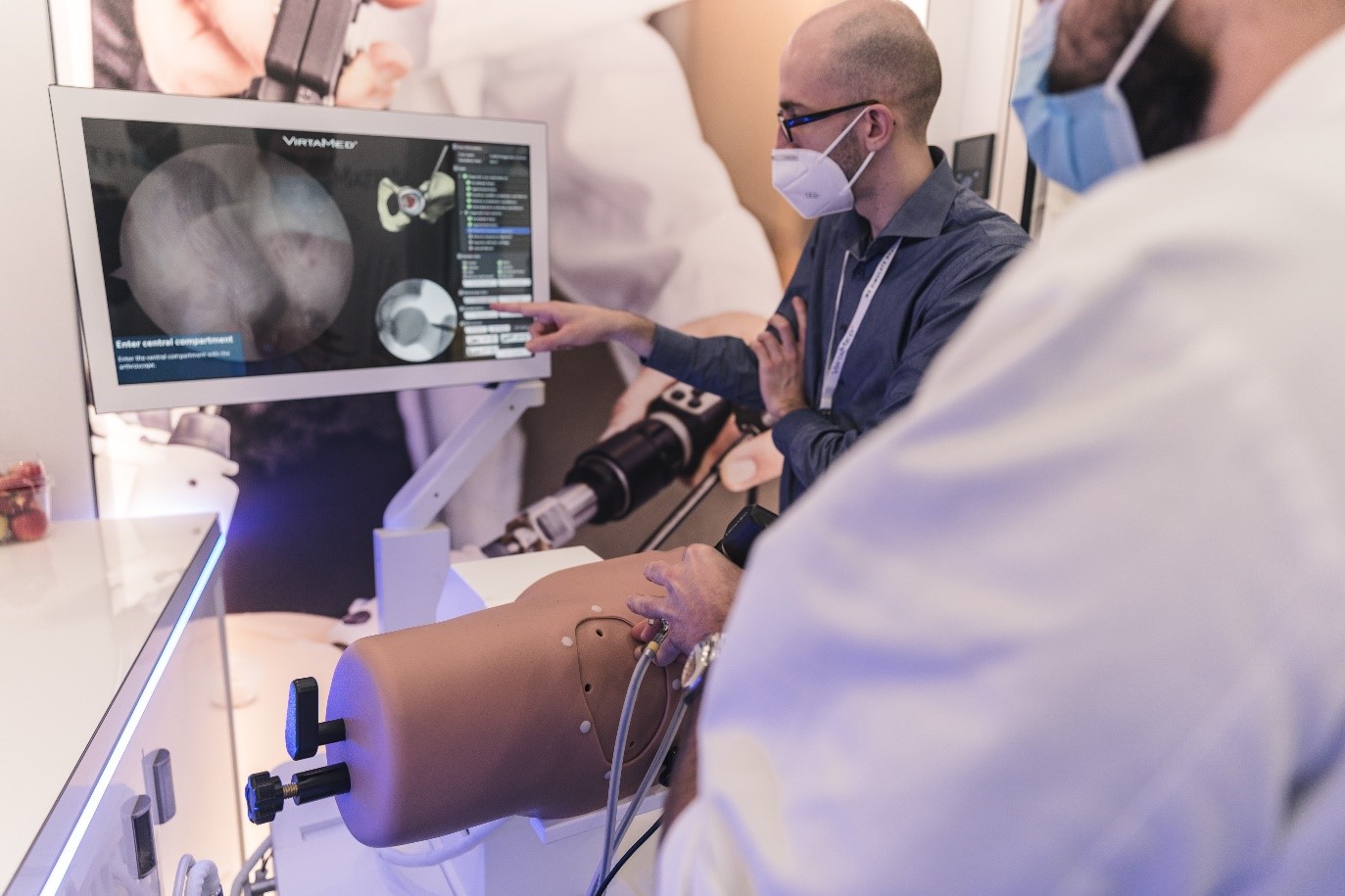
One component of this paradigm shift is virtual reality. AANA’s commitment to advancing arthroscopic training through simulation is highlighted by the exclusive and preferred partnership with VirtaMed for virtual reality simulation training. Many Orthopaedic Surgeons have benefitted from training on VirtaMed ArthroS™ simulators for knee, shoulder and hip arthroscopy, as well as a virtual reality version of the FAST training program. These simulators provide lifelike haptic feedback by combining anatomically correct rubber models with original surgical instruments, and photorealistic graphics simulate (virtual) arthroscopic and fluoroscopic views. Advanced therapeutic procedures now include rotator cuff repair, developed in partnership with Smith+Nephew.
“We believe that realistic training with objective feedback metrics is an essential element in the journey towards being proficient in the operating room,” said Stefan Tuchschmid, Ph.D., Co-CEO and Founder of VirtaMed. “Together with AANA we are able to extend our wide range of diagnostic and therapeutic training cases that can be accessed on demand and repeated to proficiency.”
A fleet of these high-fidelity simulators have been available at the Orthopaedic Learning Center (OLC) in Rosemont, Illinois since 2018, and residents from over half of orthopaedic residency programs across the United States have already used these simulators. AANA and VirtaMed work together to advance and improve the training of arthroscopic skills by leveraging the latest virtual reality simulation technology and AANA’s expertise in arthroscopy education.
“The COVID-19 pandemic has helped us improve the ultimate training we will offer,” said Joseph Tauro, M.D., AANA Board Member and Learning Center Committee Chair. Being instrumental to AANA’s start-up with virtual reality training, Dr. Tauro added, “We have been concentrating on the development of online training as a precursor to the simulation lab, focused on teaching cognitive skills that can then be built on in the lab. We are also working toward the development of more portable simulators which we can deploy across the country and internationally.”
AANA is further adding to its simulation options with a recent immersive virtual reality event, sponsored in partnership with CONMED and PrecisionOS, “OR in VR: LIVE Hip Arthroscopy in Virtual Reality,” where participants were able to experience best practices in hip arthroscopy entirely in virtual reality on a mobile wireless device (goggles).
“Immersive virtual reality (iVR) offers an opportunity for the learner to engage in the entire surgical experience. This includes triangulation, addressing multiple pathologies and using the C-arm (with no radiation), all while deciding on the limb position,” said Danny Goel, M.D., with PrecisionOS. “As a portable solution with collaborative features, it connects mentors and mentees without geographic limitation. Importantly, it also captures unique performance metrics revealing how this cutting-edge technology may present a potential paradigm shift in surgical education.”
Additionally, the ACGME is laying the groundwork to move residency programs toward using observable Entrustable Professional Activities (EPAs) as a core part of resident competency assessment. In orthopaedics, this would translate into a Proficiency-Based Progression (PBP) model. PBP training is an approach in which the trainee must acquire and demonstrate basic skill sets before progressing on to more advanced techniques. At the core of the curriculum are unambiguously defined metrics that include steps (tasks to complete) and errors (deviations from optimal performance), derived from a careful task deconstruction of the procedure (or set of skills to be mastered) by experienced practitioners.
AANA has also taken great strides in advancing a PBP training program. “AANA committed to a validated PBP training program over 10 years ago and has devoted considerable resources to make the program a reality,” said AANA Past President Louis McIntyre, M.D. “In September 2019, AANA sponsored the first proficiency-based shoulder lab at the OLC which we hope will serve as a model for future courses.”
The AANA Copernicus Initiative was a four-year series of research studies investigating the merit and impact of the PBP training model. A prospective, randomized and blinded trial was conducted to train for an arthroscopic Bankart repair and demonstrated that Orthopaedic Residents randomized to the PBP curriculum completed significantly more tasks and enacted 55% fewer errors than comparable level residents who underwent traditional training. The PBP group was also five-seven times more likely to achieve the proficiency benchmark than the control group.
The striking results of research that took place because of the Copernicus Initiative represent the need for a paradigm shift in surgical skills training from the apprenticeship to the PBP training model. AANA Past President Richard Angelo, M.D., Ph.D., commented, “The results of the Copernicus Initiative are unequivocal – there is a methodology to train surgical skills far superior to the manner in which we have done so in the past. The challenge before us is to incorporate the principles of PBP training into all of our skills training curriculums as soon as it’s feasible.” These metric-based assessment strategies could be employed to establish an appropriate barrier to entry thresholds in which the scope of practice and competency issues are a potential concern. For example, board certification for general surgery requires an acceptable performance on a laparoscopy simulator. There is a need for a similar program that requires demonstration of proficiency on an arthroscopy simulator for board certification in orthopaedic surgery.
The initiatives and models described above are all advances in simulation and arthroscopy education, and it’s exciting to think about where arthroscopy and simulation will go in the next several years and beyond, and the myriad ways AANA will assist in those advancements.


