Innovation and Adaptation of New Technology in Orthopaedics
By: Harris S. Slone, M.D., FAANA Member, AANA Communications and Technology Committee
Orthopaedics is undergoing a transformative technology epoch, most especially within arthroscopic surgery, which is distinguished by innovations, novel surgical techniques and advancements in minimally invasive surgical instrumentation. The process around development and subsequent adaptation of new technology are of great interest to many who are practicing arthroscopy and minimally invasive surgery. There have been numerous seminal technological breakthroughs that have fundamentally reshaped the landscape of orthopaedic practice as it stands today.
My interest in exploring the assimilation of emerging technologies began when developing when creating content for the AANA social medial platforms, particularly in relation to the development and implementation of arthroscopic surgery, and the history of AANA. Initially met with skepticism from the academic community, the advent of the arthroscope was not universally embraced. Famously, Dr. Charles Rockwood referred to the arthroscope as “a tool of the devil.” In response to such reservations, the International Arthroscopy Association was formed, and eventually spawned the Arthroscopy Association of North America in efforts to educate Orthopaedic Surgeons on arthroscopic techniques deemed “unlikely to succeed” by academicians.1
Many scholars have dedicated their whole careers to the study of technological advancement and innovation. Clayton Christenson authored the book 'The Innovator's Dilemma,' in which he famously describes two basic types of innovation: sustaining and disruptive.2 Sustaining innovation operates within established markets, with iterative changes and advancements. In other words, sustaining innovation is generally in response to the customer demand. Within orthopaedics, the progression towards smaller and stronger suture anchors, the introduction of highly crosslinked polyethylene, and instrumentation for minimally invasive plate osteosynthesis, are examples of sustaining innovation. While sustaining innovation predominates, it is often disruptive technology that is most impactful to a given field. Disruptive technology, epitomized by the advent of the arthroscope, isn’t developed in response to customer demand because the market for these products does not yet exist.
The development of technology does not guarantee its widespread adoption. In fact, most new technology startup companies fail to gain significant market share. The adoption of new technology is also something that has been extensively researched. In 1956, George Beal and Joe Bohlen published a paper entitled “The Diffusion Process.”3 In this fascinating study, the authors describe the processes that drive innovation and categorize adaptation of new technology amongst farmers across the United States. Despite few similarities between farming and orthopaedic surgery, their description of adaptation of new technology is very applicable to our field. They describe the “stages of diffusion,” which is essentially the evolution of knowledge and interest for a given technology. The first phase is the “awareness phase” where a person becomes aware of new technology, but no details regarding the topic. The “interest stage” is when a person wants more information regarding a topic and makes efforts to gain knowledge. The “evaluation stage” is when someone makes a critical assessment of how this new technology will affect practice. This may include financial and/or time considerations or outcomes-based assessment. The next phase is the “trial phase” where someone will venture into small scale experimental use. A person may try the new technology in different settings or with small variations in the way the new technology is used. Lastly, the “adoption phase” is when a person transitions to regular wide-scale, sustained use.
In their article, Beal and Bohlen also described the phases of adoption of new technology in farmers. Many of us are familiar with this concept of innovators, early adopters, early majority, majority and non-adopters (Figure 1) as it applies to adoption of orthopaedic technology.3
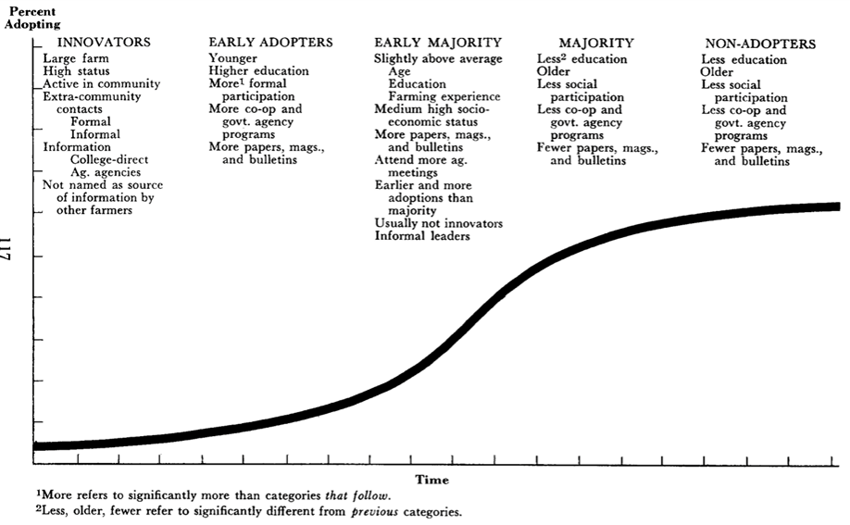
Figure 1: Beal, C.M. and Bohlen, J.M. 1956. DOI: 10.22004/ag.econ.17351
The “tipping point” in the adaptation of new technology refers to the moment in time at which interest and demand for a product or idea (or in orthopaedics a tool or surgical technique) exceeds the demand for old technology with widespread adoption, and sometimes abandonment of old technology. Malcom Gladwell describes this concept in depth in his classic 2002 book “The Tipping Point: How Little Things Can Make a Big Difference.”4 One of the main concepts of this book is that products or ideas that are not “sticky” or possess value will never reach the tipping point. This “tipping point” concept is reflected in the transition from early adopters to majority adoption as described by Beal and Bohlen (Figure 1). Another concept of Gladwell’s book is “The Law of the Few.” This refers to the concept that to reach the tipping point, a small influential group of people who are effective in spreading information about a topic is required (or in our case researching and teaching arthroscopy). It is apparent to me that this “Law of the Few” clearly reflects the godfathers of arthroscopy and many of our early AANA members.
In thinking about other factors that have influence the adaptation of new technology, medical research clearly drives clinical practice. Drs. Lubowitz, Brand and Rossi recently posed the question, 'What is the purpose of medical research?' and deemed the ultimate purpose of medical publishing to be 'practice-changing innovation.’5 Unquestionably, the quantity and quality of research, and thanks to electronic advancements, the ability to easily and immediately exchange information, ideas and results influence the adaptation of technology. In the case of arthroscopic surgery, the number of scientific publications regarding arthroscopy exponentially increased since the 1970’s (Figure 2). Based off the chart below, it appears the “tipping point” of arthroscopy occurred in the late 1990’s or early 2000’s.
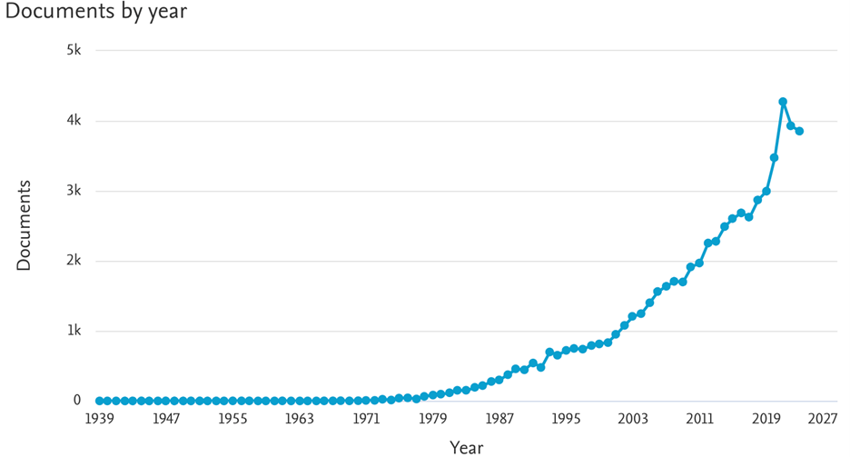
Figure 2: Source - Scopus (TITLE-ABS-KEY (arthroscopy) OR TITLE-ABS-KEY (arthroscopic))
Dr. Steve Burkhart has likely influenced modern arthroscopic shoulder surgery as much as anyone. Dr. Burkhart’s background in engineering allowed him to observe solutions to problems outside of orthopaedics and translate them to solutions for orthopaedics, and specifically arthroscopic needs. This has been referred to as “lateral thinking.”6 Dr. Burkhart has helped design numerous products commonly used today including friction-based knotless suture anchors, tape suture for improving tissue-suture properties and suture passers to name a few. Not only is Dr. Burkhart an innovator, but he is a student of innovation and adaptation of new technology. In his 2015 publication he described “The Burden of Our Craft” as it related to arthroscopic surgery.7 Surgeons are craftspeople, and the disruptive technology of arthroscopy would not have evolved into its current state without advancement of our technical skill as users of the tool. In other words, the disruptive technology of the arthroscope made things in some ways much harder, and it is our burden as surgeons to advance our skills with the adaptation of new technology. Rotator cuff repair – a surgery that many had mastered, initially took longer and was much more technically demanding when done arthroscopically versus open. Now, many trainees have never even seen an open cuff repair. Similarly, Dr. Burkhart recognizes that with new technology, one surgeon’s experience may be very different than another’s, as the skill of their craft may not be equal. The “burden” of arthroscopy was/is to develop terminology, instrumentation, surgical techniques, but also to educate and train those who require this specialized skillset.6
Dr. Burkhart identifies something that other authors in my readings on this topic fail to stress – tenacity. He describes tenacity as the invisible engine that drives innovation and disruptive change.6 In thoughtful review of the disruptive innovators in orthopaedics over the last 100 years, tenacity is unquestionably a unifying characteristic. Perhaps tenacity is the most important quality of an innovator.
Sir John Charnley who is largely regarded as the father of modern hip arthroplasty was tenacious in his study and pursuit of a better hip arthroplasty system in the 1950’s and 1960’s. Dr. Charney implanted 300 Polyte-trafluoroethylene (PTFE) acetabular components, all of which required revision due to adverse wear properties. His assistant, Harry Craven proposed a new material – compression molded ultra-high molecular weight polyethylene (UHMWPE); however, given his prior untoward experience with a similar material, Dr. Charnley concluded “we don’t want polyethylene, it’s no good” and instructed Mr. Craven to abandon the concept. Fortunately, Mr. Craven shared his mentor's tenacity and studied UHMWPE despite instructions to the contrary. When presented with early test results, Dr. Charney recognized UHMWPE was the future of low-friction hip arthroplasty and revolutionized care for hip arthritis.8
In summary, the concept of innovation and adaptation of new technology is complex and ever evolving. Innovators will fail and must be tenacious. Headwinds against the development of new technology are often strong and multifactorial. Despite all of this, we owe it to our patients through scientific study to pursue these tools and techniques that have and will continue to advance arthroscopy and minimally invasive surgery.
References
- The History of AANA. https://www.aana.org/about-aana/history-of-aana/.
- Christensen, C.M. The Innovator’s Dilemma: When New Technologies Cause Great Firms to Fail. Harvard Business Review Press; 2013.
- Beal, G.M., Bohlen, J.M. (1956). The Diffusion Process. Increasing Understanding of Public Problems and Policies.
- Gladwell, M. The Tipping Point: How Little Things Can Make a Difference. Boston: Back Bay Books / Little, Brown and Company; 2019.
- Lubowitz, J.H., Brand, J.C., Rossi, M.J. The Ultimate Goal of Medical Publishing is Practice-Changing Innovation. Arthrosc J Arthrosc Relat Surg. 2024;40(1):1-2. doi:10.1016/j.arthro.2023.10.002
- Burkhart, S.S. The Basis of Innovation: Depth, Breadth, and Tenacity. Arthrosc J Arthrosc Relat Surg. 2020;36(6):1503-1507. doi:10.1016/j.arthro.2020.04.014
- Burkhart, S.S. The Burden of Craft in Arthroscopic Rotator Cuff Repair: Where We Have Been and Where We Are Going. Am J Orthop. 2015 Aug;44(8):353-8. PMID: 26251931
- Metcalfe, R.G., Porter, M. John Charnley’s Assistant: Harry Craven and the Charnley Hip. Biomed Mater Devices. Published online February 13, 2024. doi:10.1007/s44174-024-00157-5


